I hadn't realized that I had not posted her death. She died of respiratory failure. She had fluid in her lungs and however that worked, her heart stopped. We were going to give her oxygen and take her to the ER but she died before we could leave the house.
 |
| Katharine Hepburn |
She had gone to the ER after her seizure January 27; then to the vet hospital January 28. She was there until Wednesday Jan. 31 when she came home. She was weak, couldn't-and never did-cry or make a sound. She could barely walk. The hospital said they didn't know why and that was that. We nursed her, fed her, and she could use the litter box but wouldn't eat on her own. She finally drank water Friday. But Saturday she was breathing heavily. The ER withdrew fluid from her pleural cavity-pleural effusion-but could not account for cause. She went back that evening at 9 pm but they said there was more fluid but not enough to risk removing because it was too close to the heart. Her breathing worsened over night. I should have taken her back about 2 a.m. when her breathing rate was 48 and she had this vague expression and did not easily respond to touch or speech. I had her bundled up in a blanket next to the radiator because the ER said her body temperature was dropping. She woke me at 5:30 trying to move and I picked her up and put her into bed with me. She did not try to move. She seemed to be unaware of me. She was still breathing heavily. She woke me at 6:30 with sharp, shallow sounds but still unconscious. I should have taken her then to the ER. I hesitated. I don't know why. Then it slowed about 7:15. That's when I got my husband and we were helping her when she stopped breathing. I will never again let that happen. Yes, she was likely dying but not being able to breathe must have been uncomfortable.
We took her body for a necropsy later in the day. We received the report today, February 23, 2024. The report is inconclusive. Many things were wrong but nothing to account for the pleural effusion. No heart attack. No brain tumor. No accounting for weakness or neurological issues she had been having. No real reason for liver failure. Or why her heart stopped. She had 30ml of fluid in the pleural cavity-two tablespoons. That would have made breathing hard. But not enough to stop breathing-or so vets believe.
We are going to request a tox screen as the pathologist suggested. And I'll speak to them next week about any other tests.
NECROPSY
Gross Description
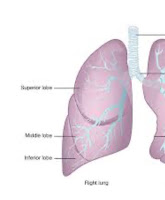
A 4.1kg spayed female cat was necropsied on 2/5/2024. Autolysis was mild. The animal had moderate amounts of subcutaneous and visceral fat, and had an overall body condition score of 6/9. Scant red-tinged fluid stained the fur around the left nares. The abdomen and left forelimb were shaved, and there was a small puncture wound over the left cephalic vein consistent with venipuncture. There was also a shaved region over the left side of thorax with needle puncture along with mild associated subcutaneous dark red hemorrhage. There were approximately 30ml of transparent, red tinged fluid ni pleural cavity. The lungs were diffusely mottled shades of dark red. The heart weighed 17g and the left and right ventricular free wals respectively measured 8mm and 3mm in thickness. There was a slightly enhanced reticular pattern. The left thyroid gland was dark purple, and enlarged measuring 2cm x 1cm x Icm; there were 3mm in diameter fluid filled cysts at the cranial and caudal ends. There were 3 blue, 1cm in diameter, spherical capsules in the stomach contents. No other significant lesions were observed.
Comments
Overall, the described changes are mild and likely incidental, or are related to clinical treatment or diagnostic procedures. The enlargement of the left thyroid gland may suggest thyroid hyperplasia or a benign tumor. No lesions to suggest any other specific underlying disease process were observed.
Microscopic Description
Representative routinely stained sections of brain, heart, lung, spleen, liver, kidney, tongue, esophagus, stomach, intestines, pancreas, urinary bladder, adrenal gland, thyroid gland, haired skin, lymph node and bone marrow were examined. Autolysis was mild.
In the left ventriculum of the heart, the cardiomyocytes were often arranged in abnormally intersecting patterns and there was variation in myofiber size. Multifocally, the myocardium was replaced by moderate amounts of fibrosis. In the lung sections, the small pulmonary vessels were occluded by fibrin thrombi.
In the liver sections, there were mild multifocal centrilobular areas of hepatocellular necrosis, characterized by loss of cellular details with retention of the architecture or loss of hepatocytes and replacement by hemorrhage. There was moderate Ito cell hyperplasia. In the pancreas, there was mild focal infiltrates of degenerate neutrophils in the pancreatic parenchyma. The peripancreatic adipose tissue was extensively replaced by amorphous basophilic to amphophilic material mixed with degenerated neutrophils, consistent with saponification.
Multifocally in the kidney section, there were mild infiltrates of lymphocytes and plasma cells in the interstitium. Rare thickened Bowman's capsules were observed. The thyroid gland were moderately hyperplastic and there was a large cyst which contained high amounts of homogeneous eosinophilic fluid in the center of the thyroid. No other significant lesions
were observed.
Morphologic Diagnosis(es)
Heart: Moderate multifocal myocardial fibrosis and myocardial disarray
Liver: Mild acute multifocal centrilobular hepatocellular necrosis
Pancreas: Mild acute neutrophilic pancreatitis with severe peripancreatic fat necrosis
Lung: Mild pulmonary thromboembolism
Thyroid gland: Moderate hyperplasia with cyst
Comments
The findings in the heart are most consistent with hypertrophic cardiomyopathy (HCM), which is the most common type of cardiac disease in cats and is a common cause of sudden death. The changes in the liver may be secondary to the cardiac condition but given the centrilobular pattern, a toxic insult cannot be completely ruled out.
The fibrin thrombi in the lung can be secondary to the heart condition or pancreatitis which can lead to disseminated intravascular coagulation (DIC). This cat also had thyroid gland hyperplasia, but this is likely non-functional and considered as an incidental finding. The findings in the kidneys are mild and likely an incidental finding as well. No further
testing is currently pending.